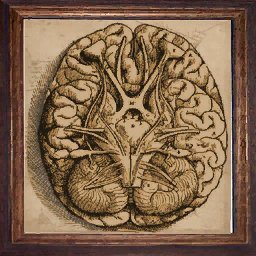
Brain
Witcher Image
|
|
Mr. Tom Jones III, a 42-year-old-man, and CEO at a Washington District of Columbia think tank was at his Georgetown home on a Sunday afternoon enjoying a cup of chicken soup. He had been feeling like he had the flu over the last two days. His sister, Ms. Kind Jones, lived across the Potomac in Arlington Virginia. Ms. Jones was looking after Tom for a few days and helping out around the house while he got to feeling a little better. Around 2 PM on Sunday, she heard Tom drop his soup; she rushed to the sitting room and found him in the midst of a seizure. Immediate she called 911. The paramedics arrived and found Tom collapsed on the floor in a semi-comatose state. Physical assessment revealed a heart rate and associated blood pressure, one pupil larger than the other, the patient was cool to touch and would utter sounds but not words. The paramedics knew Georgetown University Hospital was nearby so they decided to load him and go.
As a knowledgeable, well-trained emergency room physician, from an outstanding medical school, in Kansas City, Mr. Jones and his sister arrive in your emergency department. What do you do?
At the time of presentation in the ER, the patient is able to speak a few slightly slurred words and appears to be recovering from the seizure.
Ms. Kind Jones provides the following history: Two days ago, he woke up with a severe headache, nausea and vomited several times. A type “A” personality he never misses work but decided to stay home and that afternoon called her for help. On the phone, his speech seemed a little funny, “but I thought nothing of it, as he was not feeling well”. He stated when she arrived, something smelled funny around the house. He appeared to have lost some weight, and said he had been taking Tylenol for several weeks due to headaches. As the country was approaching the “physical cliff”, he had been thinking a lot, working on several other big projects, and attributed all his health issues to that.
Social history: No tobacco products, or illicit drugs, but doses drink socially sometimes too much.
Medications: Multivitamin, Tylenol as needed.
Surgical history: A tonsillectomy as a child.
Physical exam: A conscious, agitated, confused male, 6’1” tall weighing 185 lbs.
He had difficulty speaking much. His right pupil was slightly larger than the left. He would try to point to his nose, and mumble it “smells”. Temperature is 99.1 F, HR 120, and Respirations 20.
Neurologic exam is normal except for weakness on the left side.
|