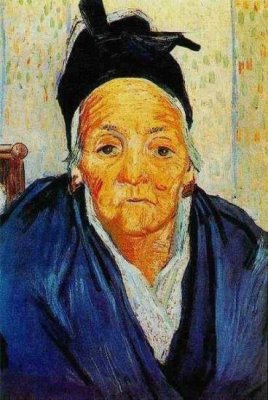
Van Gogh, "An Old Woman of Arles"
| |
Upstate New York, 2005. Winter.
An 83 year old grandmother of five presents to the ER complaining of a yellowish tint to her skin
and sclera, and
mild, intermittent, colicky pain in the right upper quadrant
of the abdomen. She reports slight weight loss over the last couple of months, and notes that her urine
has been quite dark since the jaundice began.
The grandmother reports that she is currently being treated for hypertension and hyperlipidemia.
She controls her hypertension with Atenolol, and treats her hyperlipemia via diet.
Her past surgical history is positive for a tonsillectomy and appendectomy in young adulthood.
Other than her Atenolol, she takes no other
medications. She does take a Once A Day Multi-Vitamin.
She happily tells the medical student doing her H&P that she vaginally delivered five
children in the
comfort of her own home.
She reports that she does not use alcohol or tobacco, because she is trying to set a good example for her grandchildren.
Apart from her presenting jaundice and abdominal pain, the grandmother seems to be in good spirts.
However, she does report feeling more tired than usual. She also states that her stools have been more pale than usual, and describes them as clay colored.
Physical exam reveals an elderly woman of small stature. Her skin and sclera are jaundiced.
She is alert and oriented. She has normal bowel, lung and heart sounds.
Temperature is 98.6 F, pulse 60, respiratory rate 12, blood pressure 120/80.
The liver is slightly enlarged to palpation. There are no other pertinent physical findings.
|